Blog Article
Understanding the Future of Virtual Care in Mental Health and Addiction: Results of a Recent Survey
The onset of the COVID-19 pandemic has led to a rise in virtual care solutions across various healthcare sectors. The mental health and addiction care industry is no exception to this trend. Therapists, psychiatrists, and other mental health professionals have increasingly turned to virtual telemedicine solutions to provide care to their patients in the current times of social distancing and lockdowns. However, the effectiveness of virtual care in mental health and addiction treatment continues to be a topic of debate among medical professionals and patients alike. To gain more insights into the current and future state of virtual care in mental health and addiction, we conducted a survey. In this article, we analyze the findings of our survey to help readers better understand the future of virtual care in this highly critical field of medicine.

Survey Results
We conducted our survey between August and September 2023. The survey was conducted online and collected responses from mental health professionals, patients, and caregivers. The respondents were asked about their views on virtual care, its effectiveness in providing mental health and addiction treatment, and the challenges they face.
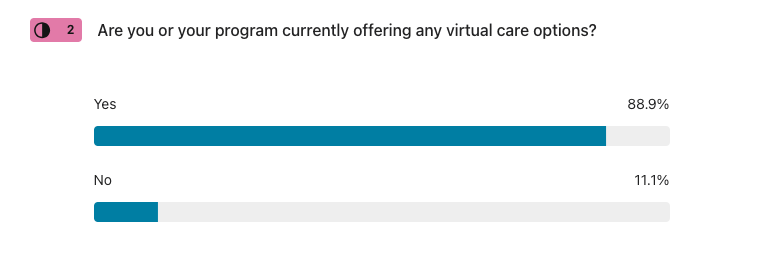
The survey found that more than 86% of the respondents were comfortable with virtual care solutions for mental health and addiction treatment and are currently offering some form of care. In fact, 68% of treatment programs offer Telehealth appointments, and at least 43% offer aftercare, family support, or virtual intensive outpatient services.

While some 11% of respondents do not currently offer virtual care options, 100% indicated they intend to offer options in the near future.
Most respondents believed that virtual care is effective in improving outcomes, with 88% of professionals reporting that the greatest benefit is better education for wellness. This was followed by more flexible access to care at 94%, extended connection to treatment and better access to support groups at 89%. However, despite these positive perceptions, a large portion of the respondents mentioned that they believed virtual care cannot always replace in-person care delivery, especially in more severe cases or based on the drug of choice.

One of the biggest challenges identified in virtual care delivery was the issue of privacy and security of patient information. Almost 40% of the respondents expressed their concerns about data confidentiality and security in virtual care delivery. Other significant challenges identified were a lack of non-verbal cues communication during virtual sessions, resource management, lack of access to stable internet connections, and technological challenges with platforms.
87% of healthcare professionals who responded to the survey plan to continue providing virtual care or begin offering solutions. They believe that virtual care has many benefits, including increased access, convenience, and flexibility.
Another portion of our survey dove into how beneficial the respondents found virtual care to be in different aspects of their mental health and addiction treatment programs.
When it came to increased revenue, 61% found that virtual care would be beneficial to their existing programs. Virtual care can enhance revenue streams for treatment centers in several ways. Primarily, it allows them to serve more patients, including those beyond their geographical location, and offers flexibility in scheduling, which can potentially lead to a higher number of billable hours.
For increasing their connection to patients, 78% found it beneficial. Virtual care provides an increased connection to patients by breaking down geographical barriers, enabling therapists and professionals to reach and treat individuals who may not have access to these services.
In terms of differentiating the services they offer, none of the respondents found virtual care to be not beneficial. However, a striking 39% remained neutral on the impact, with 22% finding it somewhat beneficial and 39% acknowledging it as very beneficial.
The perception of virtual care in improving patient outcomes was more polarized. While no one found it not beneficial, 17% rated it not very beneficial. However, the majority leaned towards beneficial with 83%.
Finally, in terms of increasing efficiency for themselves or their staff, none of the respondents found virtual care to not be beneficial. A minority of 5.6% found it not very beneficial, another 5.6% remained neutral, while the majority 89% found it to be beneficial to their organizations.

These results demonstrate that, while there are differing opinions on the benefits of virtual care, the majority of respondents find it at least somewhat beneficial in various aspects of mental health and addiction treatment.
In the next part of our survey, we asked treatment centers about their perceptions of patient concerns regarding the use of virtual care. A range of concerns were identified by respondents. The most commonly raised issues were related to technology, with respondents specifically noting concerns about patients' access to necessary hardware, computer equipment, and stable internet connections.
Several respondents pointed out concerns about the privacy and confidentiality of information during virtual sessions. The inability to obtain medications other than pharmacy redirects, and patients' levels of engagement with caregivers in a virtual setting were also highlighted as potential issues.
Moreover, respondents worried about patients feeling less connected in a virtual environment. It was suggested that an in-person therapeutic alliance should ideally be established before transitioning to virtual care. The lack of face-to-face interaction and the impersonal nature of virtual sessions were also mentioned as potential patient concerns.
A significant concern raised was the authenticity of virtual care-some respondents felt it wasn't seen as "real" treatment. One respondent emphasized that virtual care could eliminate the core interpersonal aspect of therapy and felt that it should not be the norm but rather an extension of in-person treatment.
Finally, there were concerns about patients managing increased screen time, the lack of confidence in using technology, and the risk of exacerbating feelings of disconnection and isolation in an already disconnected world. Some respondents insisted on the necessity of in-person treatment components and voiced concerns about promoting virtual care. Interestingly, one response indicated that they believed there were no concerns at all about patients participating in virtual care.
The survey respondents shared diverse concerns about the provision of virtual care. These encompassed various areas, including privacy and confidentiality of information, technology-related issues, and the potential loss of human connection in a virtual setting. Some respondents pointed out issues related to substance use disorders. They noted that patients might shortcut their path to obtain 'comfort meds' and expressed skepticism about progress to recovery through telemedicine.
A recurring theme in the responses was disparities in access to care across large catchment areas. Concerns about safety and stricter admission criteria for serious cases were also mentioned. Some respondents highlighted that unless a trusting in-person relationship has been established, the benefits of virtual care could be minimal. Technical glitches, such as internet or power outages, were seen as potential barriers to effective care delivery.
The survey also revealed concerns about funding and the added burden of managing an additional system. A few respondents expressed their concerns over the reduced efficacy of interventions and a decrease in the quality of therapeutic connections. They felt that the seriousness with which clients attended virtual appointments was inferior to in-person visits. Despite these concerns, it is noteworthy that some respondents were already providing care virtually, indicating a level of adaptation and acceptance of this new mode of care delivery.
Conclusion
The survey results indicate that virtual care has become an important part of mental health and addiction care delivery. It is an effective alternative to in-person care and has helped many patients improve their mental health outcomes. However, while virtual care has numerous advantages, some challenges remain, such as privacy and security concerns, technological issues, and a perceived inability to replace in-person care for severe cases. Our survey suggests that virtual care will continue to grow and it has become an integral part of providing care. However, it is imperative to address the identified concerns to ensure that virtual care is delivered safely, beneficially, and effectively in mental health and addiction care.
If you or someone you know is navigating the complexities of mental health issues or addiction, Interact Lifeline is here to help. We are committed to providing easily accessible, effective, and affordable treatment options. Don't let geographical constraints or societal stigma deter you from seeking the help you deserve. Reach out to us for more information about our digital mental health and addiction treatment services. Your path to recovery can start today. Connect with us at Interact Lifeline, and let's take the first step towards healing together.
Get Started with InterAct LifeLine
InterAct connects individuals to treatment, support
communities & families to improve recovery.
